Conjugated Oestrogens
Conjugated Oestrogens
- In our pharmacy, you can buy conjugated oestrogens without a prescription, with delivery in 5–14 days throughout the United Kingdom. Discreet and anonymous packaging.
- Conjugated oestrogens are used for the relief of menopausal symptoms such as vasomotor symptoms and vaginal atrophy. They work by supplementing the body’s oestrogen levels.
- The usual dosage for menopausal symptoms is 0.3–0.625 mg taken once daily.
- The form of administration is an oral tablet or vaginal cream.
- The effect of the medication begins within a few hours, depending on the form used.
- The duration of action is approximately 24 hours for oral tablets.
- Alcohol consumption should be limited as it may increase the risk of side effects.
- The most common side effect is breast tenderness or pain.
- Would you like to try conjugated oestrogens without a prescription?
Basic Conjugated Oestrogens Information
- INN (International Nonproprietary Name): Conjugated estrogens
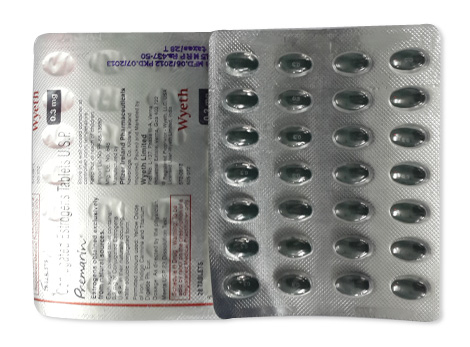
- Brand Names Available in United Kingdom: Premarin®, Premique®, Prempak-C®
- ATC Code: G03CA57
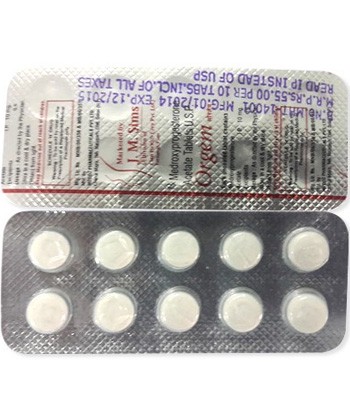
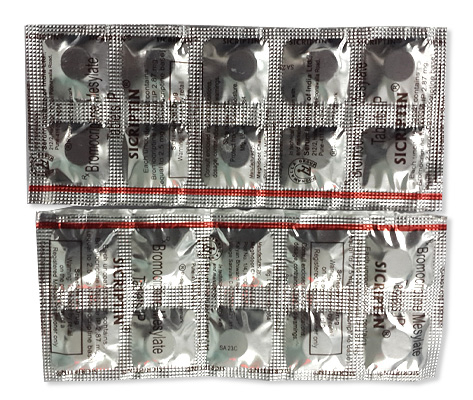
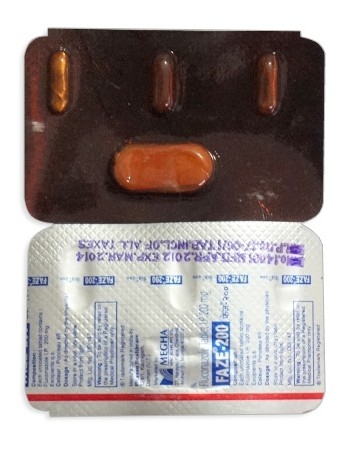
- Forms & Dosages: Oral tablets (0.3 mg, 0.625 mg, 1.25 mg), vaginal creams (0.625 mg/g)
- Manufacturers in United Kingdom: Pfizer
- Registration Status in United Kingdom: Licensed
- OTC / Rx Classification: Prescription-only (Rx)
Everyday Use & Best Practices
When considering the use of conjugated oestrogens, timing doses effectively can be crucial for maximising benefits. Many practitioners suggest aligning dosing schedules with the body's natural hormone cycles. For instance, taking medication in the morning might be advantageous for those experiencing early-day symptoms, while evening doses can help manage discomfort at night.
It's also essential to take personal schedules and preferences into account. Balancing lifestyle and medication routines ensures adherence, which is vital for the effectiveness of any hormone therapy.
Taking With or Without Meals
In the context of UK dietary habits, patients might wonder whether to take conjugated oestrogens with food or on an empty stomach. Generally, it is advisable to take these medications consistently—either always with meals or always without. Taking doses with food can help prevent potential stomach upset, while an empty stomach might enhance absorption for some individuals.
UK diet habits, rich in fibre and varied in types of food consumed, can influence how well the medication is absorbed. For instance, high-fat meals may affect the body's absorption of certain hormones, so understanding one's typical diet can guide when to take conjugated oestrogens most effectively.
Safety Priorities
According to the Medicines and Healthcare products Regulatory Agency (MHRA), there are specific populations that should consider avoiding conjugated oestrogens. Those with a history of certain cancers, particularly hormone-sensitive cancers, or with clotting disorders may be at higher risk. Additionally, women who have unusual bleeding patterns should seek medical advice before commencing treatment.
Understanding these safety priorities is critical in making informed healthcare decisions. Regular consultations with healthcare providers are essential for managing risks effectively.
Activities to Limit
Potential side effects from using conjugated oestrogens could impact daily activities, especially for those prone to dizziness or fatigue. Caution is advised when undertaking tasks that require full concentration, such as driving or operating heavy machinery. Individuals should assess how they feel after starting treatment before resuming these activities.
Listening to one's body and recognising when to take a break from demanding activities can help manage side effects effectively.
Dosage & Adjustments
Standard dosing for conjugated oestrogens is typically guided by NHS recommendations. Generally, a starting dosage for menopausal symptoms can range from 0.3 to 0.625 mg daily, which may be adjusted based on individual response and effectiveness. Available forms include oral tablets and vaginal creams, which provide flexibility in administration routes.
Tailoring dosage for specific populations is vital. Elderly patients, for example, may require lower doses due to heightened risks associated with hormone therapy. Similarly, those with pre-existing conditions should have their dosages assessed and adjusted by healthcare professionals to ensure safety.
Special Cases
When dealing with conjugated oestrogens, personal health conditions can necessitate dosage modifications. For elderly patients, initiating treatment at the lowest effective dose is usually advised due to the increased risk of thromboembolic events. Concurrent health issues, such as liver or kidney impairments, require careful monitoring and, in some cases, dosage adjustments to maintain therapeutic efficacy while minimising risks.
Regular reviews with healthcare providers ensure that any changes in health status are reflected in treatment plans.
User Testimonials
Many patients in the UK have shared positive experiences while using conjugated oestrogens, finding relief from symptoms associated with menopause and hormonal imbalances. Anecdotal reports highlight significant improvements in quality of life, particularly concerning hot flashes and mood swings.
However, common challenges have emerged from community forums, with some individuals reporting side effects such as bloating or breast tenderness. These findings underscore the importance of ongoing communication with healthcare providers to navigate treatment effectively.
Buying Guide
Purchasing conjugated oestrogens is a straightforward process for most individuals in the UK. Pharmacies such as Boots, LloydsPharmacy, and Superdrug offer these medications. It's possible to buy conjugated oestrogens without a prescription in certain circumstances, highlighting the accessibility of this treatment.
Price comparisons reveal significant variations between NHS prescription charges and private purchases. Patients should evaluate their options based on personal financial situations and available healthcare plans, as being informed can lead to better choices for long-term health management.
What’s Inside & How It Works
Ingredients overview
Conjugated oestrogens, primarily sourced from the urine of pregnant mares, contain a blend of various active estrogen compounds aimed at managing menopausal symptoms.
Key active ingredients often include:
- Estrone sulfate
- Equilin
- Equilenin
- Other sulfonated estrogens
In addition to the active compounds, conjugated oestrogens may contain excipients such as:
- Lactose
- Magnesium stearate
- Starch
These components work together to ensure optimal absorption and stability, enhancing the therapeutic effects for users.
Mechanism basics explained simply
Conjugated oestrogens effectively counter menopause-related symptoms by mimicking the action of natural estrogen in the body. During menopause, hormonal levels decline, leading to various uncomfortable symptoms such as hot flashes and vaginal dryness.
By replenishing estrogen levels, these compounds work to:
- Regulate body temperature, reducing hot flashes
- Maintain vaginal health and moisture
- Support bone density, decreasing the risk of osteoporosis
In essence, conjugated oestrogens provide a crucial hormone replacement during a transitional phase in a woman's life, promoting comfort and well-being.
Main Indications
Approved uses (MHRA listing)
Conjugated oestrogens hold several approved uses, adhering to the guidelines set out by the MHRA:
- Management of menopausal symptoms, including hot flashes and vaginal dryness
- Prevention of osteoporosis in postmenopausal women
- Treatment of hypoestrogenism in women with primary ovarian insufficiency
They act as essential remedies for women experiencing the multifaceted challenges associated with menopause.
Off-label uses in UK clinics
While conjugated oestrogens are predominantly used for the indications mentioned, they are occasionally prescribed off-label in UK clinics. Some potential off-label uses include:
- Treatment of certain types of breast and prostate cancers
- Management of endometriosis-related symptoms
- Approaches to chronic fatigue syndrome among some patients
This expanded use highlights the versatile nature of conjugated oestrogens and illustrates healthcare professionals' adaptability in managing different health conditions.
Interaction Warnings
Food interactions (alcohol, tea/coffee)
Diet can significantly affect the effectiveness of conjugated oestrogens. It's vital to be mindful of interactions with specific foods and drinks:
- Alcohol may elevate the risk of side effects, such as liver complications
- Caffeinated beverages like tea and coffee can interfere with hormone metabolism
Thus, moderation is key, and discussing dietary choices with a healthcare provider can optimise treatment outcomes.
Drug conflicts (MHRA Yellow Card reports)
Drug interactions can pose risks while using conjugated oestrogens. Common medications that may conflict include:
- Anticoagulants and anticoagulant therapy
- Certain antibiotics that may affect hormone levels
- Medications for seizures
Patients should consult their healthcare providers for personalised advice before starting treatment. Highlighting these interactions leads to a more safe and effective treatment experience.
Latest Evidence & Insights
Recent studies conducted within the UK and EU from 2022 to 2025 have shed light on the efficacy and safety of conjugated oestrogens. Research has demonstrated benefits in managing menopausal symptoms, with particular attention to the balance of benefits versus risks over long-term use. Some pivotal findings include:
- Improvement in overall quality of life measures among women
- Research into long-term cardiovascular health outcomes, revealing no significant adverse cardiovascular effects
- Studies indicating minimal risk for certain cancers when under medical supervision
These insights suggest that conjugated oestrogens can be a beneficial component of hormone replacement therapy for menopausal women, especially when personalised approaches to treatment are employed.
Alternative Choices
For those seeking different options for managing menopausal symptoms often addressed by conjugated oestrogens, the NHS provides several alternative therapies.
Here’s a concise look at some alternatives, with a checklist of their pros and cons:
- Selective Estrogen Receptor Modulators (SERMs):
- Pros: Target specific tissues, potentially fewer side effects.
- Cons: Not as effective for all symptoms, may still require estrogen.
- Phytoestrogens (natural plant hormones):
- Pros: Generally considered safe and well-tolerated.
- Cons: Limited evidence on long-term efficacy.
- Hormonal Alternatives (Estradiol, Tibolone):
- Pros: Other hormonal options with specific mechanisms of action.
- Cons: Risk of similar side effects as conjugated oestrogens.
- Non-Hormonal Therapies (SSRIs, SNRIs):
- Pros: Effective for mood swings and hot flashes.
- Cons: May not address all menopausal symptoms, side effects possible.
Ultimately, each therapy presents unique advantages and challenges. It's vital to have a conversation with a healthcare provider to find the most suitable option.
Regulation Snapshot
The Medicines and Healthcare products Regulatory Agency (MHRA) plays a critical role in the approval process for medications in the UK, including conjugated oestrogens. This regulatory body ensures that all medications meet strict safety and efficacy standards before they can be prescribed.
Before a drug can be included in NHS prescribing, it undergoes several stages of assessment. The process evaluates factors like the quality, safety, and effectiveness of the medication. Following approval by MHRA, the Clinical Commissioning Groups (CCGs) may decide on the drug's availability within local health services.
This thorough oversight ensures that only effective treatments reach patients, aligning with NHS guidelines. Enhanced safety monitoring continues even after medications are approved, providing an extra layer of confidence for prescribers and patients alike.
FAQ Section
Here are some common questions UK patients might have about the use of conjugated oestrogens:
1. What are conjugated oestrogens used for?
They are primarily used to treat menopausal symptoms like hot flashes and vaginal dryness.
2. Are there any risks associated with taking conjugated oestrogens?
Yes, potential risks include blood clots and certain types of cancer. It’s important to discuss personal risk factors with a healthcare provider.
3. How long can I use conjugated oestrogens?
Usage should be reviewed regularly, typically every 3-6 months, to assess the need for continuation or dose adjustments.
4. Can I buy conjugated oestrogens without a prescription?
In the UK, they are classified as prescription-only medication, which means a prescription from a doctor is typically required.
Guidelines for Proper Use
UK pharmacist counselling style
During consultations, patients can expect pharmacists to provide tailored guidance about using conjugated oestrogens. This often includes:
- An overview of how to take the medication, including timing and dosage.
- Advice on common side effects and what to do if they occur.
- Information on missed doses and what steps to take.
- Encouragement to share any pre-existing conditions or medications that may interact.
Engaging in open dialogue with the pharmacist helps ensure safe and effective use of the medication.
NHS patient support advice
For those seeking further support and information about conjugated oestrogens, the NHS provides various resources, including:
- NHS Choices: Offers comprehensive information on menopause and related treatments.
- Local support groups: Many areas have support networks that encourage sharing experiences and advice.
- Patient helplines: Available to answer any immediate questions or concerns regarding medications.
Utilising these resources can significantly enhance a patient's understanding and management of their health.